|
Using protein therapeutics, clinicians try to deliver healthy proteins directly into human cells, in order to replace malfunctioning ones. Although it is considered one of the most direct and safe approaches for treating diseases, its effectiveness is limited due to low delivery efficiency and the poor stability of proteins, which are frequently broken down and digested by cells’ protease enzymes, even before they reach their intended target. Now, in a new study, a team of researchers at UCLA proposes a new method to deliver healthy proteins.
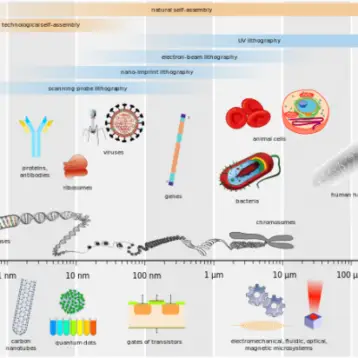
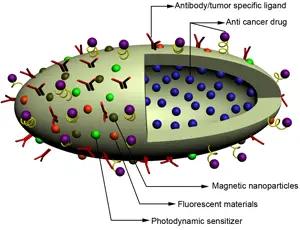
In order to create a better technique the team utilized nanotechnology to create nanocapsules – submicroscopic containers composed of an oily or aqueous core. In this case, these microcapsules contain a single protein, surrounding it with a thin, permeable polymer membrane roughly several to tens of nanometers thick. This membrane can either degrade or remain intact, depending on the size of the molecular substrates with which their embedded protein must interact, thus making the nanocapsules very effective; when degrading, the protein will transfer to nearby cells, and when intact, it will protect the protein from protease attacks as well as keep it stabilized.
“For proteins in general, it’s very difficult to cross the cell membrane. The protease will usually digest it, making stability an issue,” said lead study author Yunfeng Lu, a UCLA professor of chemical and biomolecular engineering. The aforementioned membrane improves the protein’s stability, since it makes factors such as varying temperatures and pH levels irrelevant. “Here, we’ve been able to use this new technology to stabilize the protein, making it very easy to cross the cell membrane, allowing the protein to function properly once inside the cell,” said Lu. “This is one of our biggest achievements.”
A possible drawback of a non-degradable skin is the risk of preventing substrates of larger molecular weight from reaching the embedded protein. Therefore, the skin was designed to be degradable – in order for the protein to be able to interact with a large substrate.
“Covering the protein payload with a polymeric shell provides added stability in circulation, where there are plenty of proteases to degrade the naked protein,” said Lily Wu, professor of medical and molecular pharmacology at the David Geffen School of Medicine at UCLA and an author of the study. “This will clearly be advantageous in improving efficacy of delivery.”
According to the paper, published in the January 2010 edition of the journal Nature Nanotechnology, the nanocapsule interacts with the cell when it is initially intact; initially it reacts to the endosomes – which have lower pH levels than the outside cellular environment – triggering the degradation of the polymer skin layer. Then, the protein cargo is released intracellularly.
The research also demonstrates that the skin layers can also be degraded by incorporating components which are sensitive to proteases. Using this approach, clinicians will be able to provide a more targeted delivery of the proteins. Moreover, the study shows that multiple proteins can now be delivered to cells with high efficiency and activity but low toxicity. Medical companies could manufacture various applications in protein therapies, as well as applications in the fields of vaccines, cellular imaging, tumor tracking, cancer therapies, and even cosmetics. “This new technology holds promise in all these aspects and that’s why it is so exciting to me,” Wu said.
The study was co-authored, involving Zhen Liu, a professor of chemical engineering at Tsinghua University in China, and Yi Tang and Tatiana Segura, UCLA professors of chemical and biomolecular engineering. “Right now, a lot of protein therapeutics available only act outside of the cell because it’s been difficult to deliver the proteins inside the cell,” explains Segura on the innovativeness of their research.
Although the team originally described the use of this technology with only five different proteins, now they hope it will serve as a delivery platform for all types of proteins or protein drugs. “I think the important next step is to apply this technology in a relevant, preclinical disease model. Based on the promising results of improved efficiency of delivery into cells, I anticipate improved efficacy in preclinical animal models as well,” Wu said
The team has already expanded the technique to support more than two-dozen different proteins, giving the notion that in the near future its benefits will show. “In the long run, the hope is to develop new technology that can make a difference in the lives of patients,” said Wu.
TFOT has also covered Philips’ iPill technology, which has the potential to take intelligent drug delivery to the next level, and the manner in which proteins assemble DNA sequences. Other TFOT stories that deal with futuristic medical developments include Bone Setting Glue, a piece which describes a substance that turns from a liquid to a solid as it is exposed to higher pH levels, and the Sci-Fi Future of Surgery, in the form of robots performing operations.
For more information about UCLA’s development of protein delivering nanocapsules, see the university’s website.